How multimodal treatment impacts cognitive functioning in malignant glioma patients
15th June 2020
Martin Kocher, Christiane Jockwitz, Svenja Caspers, Jan Schreiber, Ezequiel Farrher, Gabriele Stoffels, Christian Filss, Philipp Lohmann, Caroline Tscherpel, Maximilian I. Rugef, Gereon R. Fink, Nadim J. Shah, Norbert Galldiks, Karl-Josef Langen
Current treatment strategies for patients with malignant glioma usually comprise repeated and multimodal interventions, such as complete or partial tumour resections, local radiotherapy, and multiple courses of chemotherapy. The combined use of these approaches has resulted in the prolongation of survival time for a significant portion of patients. However, progressive cognitive decline following multimodal neurooncological treatment is a common observation in patients and is thought to be due to alterations in the default-mode network (DMN).
Based on investigations from a cohort of 80 patients and 80 healthy matched volunteers, the aim of this study was to analyse alterations in the DMN using resting-state functional MRI (rs-fMRI) and neuropsychological testing. For the evaluation of structural and metabolic changes after treatment, anatomical MRI and amino acid PET using O-(2-[18F]fluoroethyl)-L-tyrosine (FET) were simultaneously acquired to rs-fMRI on a hybrid MR/PET scanner.
It was found that structural tissue changes located at or near the tumour site (including resection cavities, white matter lesions, edema, and tumour tissue) had a strong negative impact on the functional connectivity of the adjacent DMN nodes, resulting in a marked dependence of the connectivity pattern on tumour location. In the majority of neurocognitive domains, glioma patients performed significantly worse than healthy subjects. Correlation analysis revealed that reduced connectivity in the left temporal and parietal DMN nodes was associated with low performance in language processing and verbal working memory. Furthermore, connectivity of the left parietal DMN node also correlated with processing speed, executive function, and verbal as well as visual working memory. Overall loss in DMN connectivity and cognitive decline was less pronounced in patients with higher education.
The results of this study imply that when planning surgery and local radiotherapy, consideration should be given to the left parietal and temporal DMN nodes, as well as the age and educational status of malignant glioma patients in order to minimize treatment-related neurocognitive deficits.
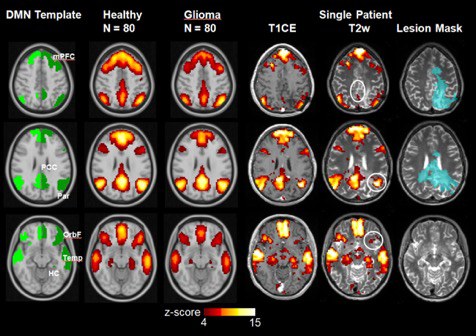
The figure above shows the default mode network (DMN) template and average DMN (z-score map) in 80 post-therapeutic glioma patients and a matched cohort of healthy subjects. The individual DMN network of a female patient with a small, multifocal recurrence with perifocal edema 10 months after first-line therapy is shown on the right. The circles in white depict the DMN-nodes with reduced connectivity. T1CE: T1-weighted MR image with contrast enhancement, PET: O-(2-[18F]fluoroethyl)-L-tyrosine Positron-Emission-Tomography, arrows: multifocal, small contrast-enhancing, PET-positive tumor nodules. DMN nodes: mPFC - medial prefrontal cortex, OrbF - orbitofrontal cortex, PCC - posterior cingulate/retrosplenial cortex, Temp - lateral temporal cortex, Par - inferior parietal lobule, HC - hippocampus/parahippocampal cortex
Original publication:
Role of the default mode resting-state network for cognitive functioning in malignant glioma patients following multimodal treatment
